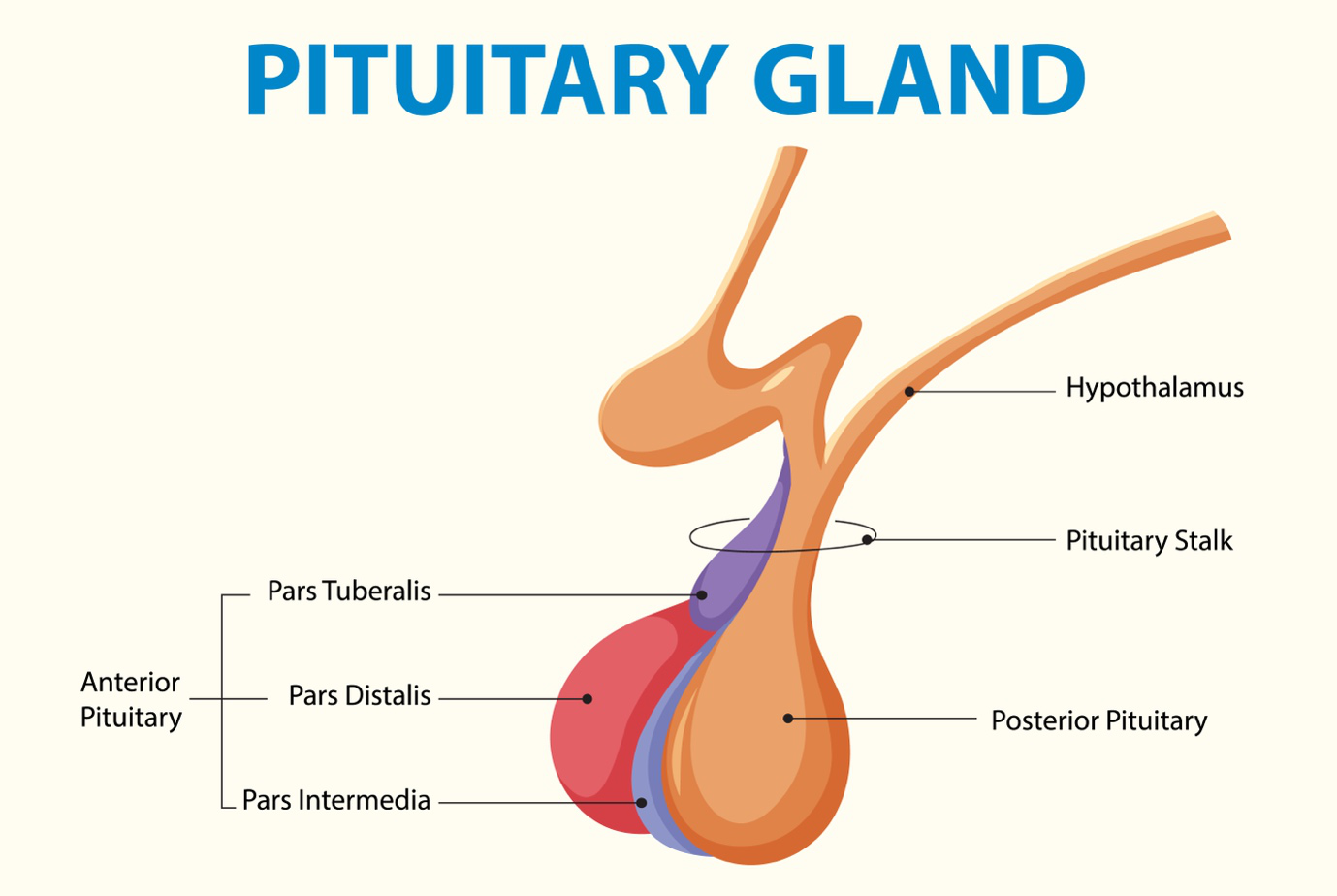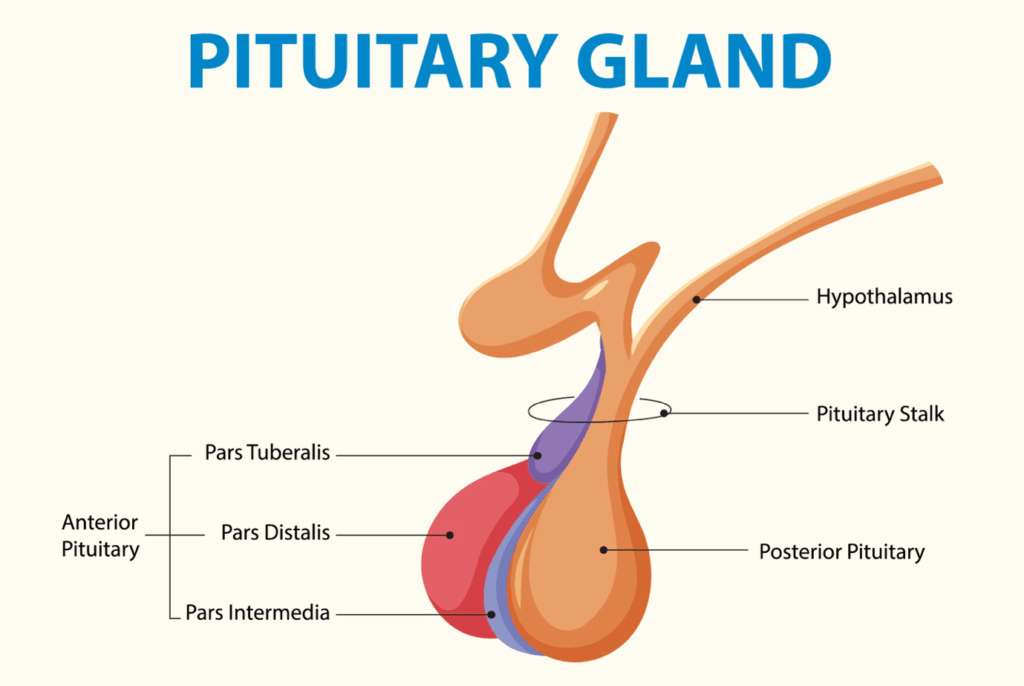
The pituitary gland, a diminutive but indispensable endocrine gland nestled at the base of the brain, plays a pivotal role in regulating a myriad of essential bodily functions. This master gland secretes a variety of hormones that govern growth, metabolism, reproduction, stress response, and fluid balance.
Pituitary tumors, abnormal growths that develop on the pituitary gland, can disrupt the delicate hormonal balance orchestrated by this gland, leading to a spectrum of health complications. While not all pituitary tumors necessitate surgical intervention, surgery remains a critical treatment modality in specific clinical scenarios.
Understanding Pituitary Tumors
Pituitary tumors are predominantly benign, i.e., they are noncancerous growths that do not typically spread to other parts of the body. However, their location and their potential to interfere with pituitary function make them a significant health concern.
Pituitary tumors are classified into two main categories, based on their hormonal activity:
- Functioning Tumors:These tumors are characterized by their ability to secrete excess amounts of one or more pituitary hormones.
- Nonfunctioning Tumors:These tumors, in contrast, do not secrete excess hormones. They may remain asymptomatic for extended periods and are often discovered incidentally during imaging studies performed for other reasons.
The Diagnostic Pathway for Pituitary Tumors
The diagnosis of a pituitary tumor typically involves a combination of clinical evaluation, hormonal testing, and advanced imaging techniques:
- Hormone Tests:Blood and urine tests are essential to measure the levels of various pituitary hormones and identify any hormonal excesses or deficiencies.
- Imaging Tests:Magnetic resonance imaging (MRI) is the gold standard imaging modality for visualizing the pituitary gland and detecting pituitary tumors.
- Vision Tests:Visual field testing is performed to assess for any visual impairments caused by compression of the optic nerves.
When Is Surgery the Answer?

The decision to pursue surgery for a pituitary tumor is a complex one, requiring careful consideration of several factors.
Surgery is typically considered when:
- The Tumor Is Causing Significant Symptoms:When the tumor is responsible for bothersome or debilitating symptoms, such as persistent headaches, vision problems, or hormonal imbalances that are not adequately controlled with medication, surgery may be recommended to alleviate these symptoms.
- The Tumor Is Compressing the Optic Nerves and Threatening Vision:Compression of the optic nerves poses a serious risk to vision. Surgery is often necessary to decompress the optic nerves and prevent or reverse vision loss.
- The Tumor Is a Functioning Tumor That Is Producing Excess Hormones:In cases where a functioning tumor is secreting excess hormones and causing significant health problems, surgery may be performed to remove the tumor and restore normal hormone levels.
Surgical Approaches to Pituitary Tumors
The surgical approach to a pituitary tumor depends on its size, location, and relationship to surrounding structures.
The two main surgical techniques are:
- Transsphenoidal Surgery:This is the most common and preferred surgical approach for most pituitary tumors. It is a minimally invasive procedure that involves accessing the pituitary gland through the nasal passages and sphenoid sinus (an air-filled space behind the nasal cavity).
- Craniotomy:In rare cases, a craniotomy, which involves opening the skull, may be necessary for very large or complex tumors that cannot be safely removed through the transsphenoidal approach.
Seeking Expert Care
If you have been diagnosed with a pituitary tumor or are experiencing symptoms that may suggest a pituitary tumor, it is important to seek evaluation and treatment from a specialized medical center with expertise in pituitary disorders.
The physicians at Houston Physicians Hospital can help.
On the page of Neurosurgery and Spine Specialist in Webster, you can scroll down and find a physician who’s right for you. Then click their link to visit their website and make an appointment.